You walk into the Consult Room and see a shy 7-year-old boy who won’t look at or make eye contact with you when you introduce yourself. Mom interjects and says, “Luke doesn’t like to smile.” You play it off and try to put Luke’s mind at ease, saying “That’s okay Luke, it’s totally normal for kids your age not to like the way their teeth look.”
You walk into the Consult Room and see a shy 7-year-old boy who won’t look at or make eye contact with you when you introduce yourself. Mom interjects and says, “Luke doesn’t like to smile.” You play it off and try to put Luke’s mind at ease, saying “That’s okay Luke, it’s totally normal for kids your age not to like the way their teeth look.”
You review Luke’s records and perform a clinical examination. He’s Class I with mild-moderate crowding, narrow arches, 4mm OJ, and mildly deep OB. You tell Mom and Luke that they’re in luck – no braces yet! You explain that while Luke will need orthodontic treatment in the future, he doesn’t need treatment now since all his problems can be corrected in one phase once most of the adult teeth have erupted.
To your surprise, instead of being happy about the news, Luke’s eyes begin to well up with tears. You thought he’d be happy about this news, so you ask, “What’s the matter Luke?” He just looks down and shrugs his shoulders. Mom covers for him and says, “He was kind of hoping that you’d say he needed braces.” “Don’t worry, you’ll have them before too long” you reply. You add that you want to see Luke back in a year so you can monitor his growth and dental development.
At that observation visit a year later, Luke won’t even talk. He just sits there with his head down, looking into his lap. He barely opens his mouth for you to look inside. You ask mom if everything is okay, and she tells you that Luke has been being bullied on the bus because of the way his teeth look. The kids call him “snags” because they say he has a snaggle tooth (tooth #7 is positioned labially). Your heart sinks. You had this little guy in your chair a year earlier and didn’t do anything to help him.
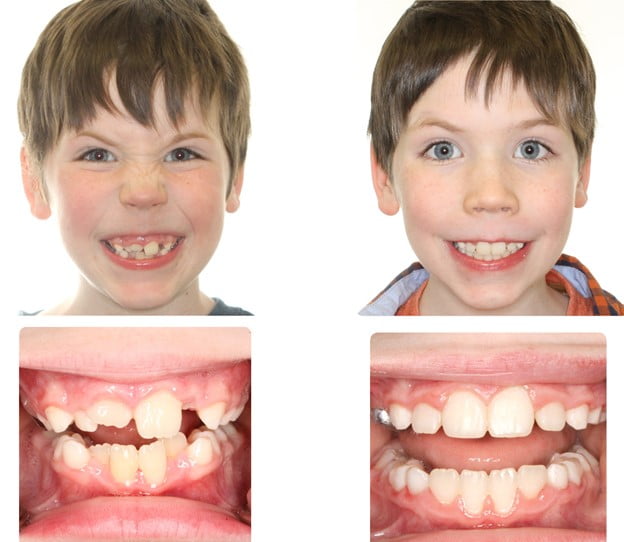
Contrast that with Emily. Emily is a 7-year-old who is in your daughter’s 1st grade class, so you know the family from seeing them at school events. Emily has the exact same malocclusion as Luke and, at the NP Exam, mom also says that Emily doesn’t like to smile. You decide to treat her with Phase I upper and lower braces to expand/develop her arches and align her teeth. Treatment proceeds as planned, and after 1 year you remove her braces. Her arches are expanded, her crowding is resolved, and her teeth and smile look AMAZING.
You run into mom and dad at a school event a few months after Emily’s debond. Mom pulls you aside to tell you that she can’t thank you enough for what you’ve done for her daughter. “Oh, you’re so welcome!” you reply, very much appreciating the kind words. “No,” mom says firmly, “you don’t understand what you did for her. Emily was getting teased about her teeth by some of the boys in her class. She would come home crying every day and say she hated school and didn’t want to go back. Every morning it was a struggle to get her on the bus.
“After she had the braces on for a few months, we started to notice a change in her. She wasn’t coming home as upset and wasn’t resisting getting out the door in the morning. And now, she’s like a totally different kid. She loves her smile and no longer gets teased about her teeth! We actually brought her to another orthodontist before coming to your office and they said she didn’t need treatment yet. I was telling one of my friends and they mentioned you were an orthodontist, so we decided to bring her to see you for a second opinion, and we are SO thankful that we did! We are beyond pleased with the entire experience!”
So I ask you, why do the majority of orthodontists treat patients using the approach taken with Luke? Why not treat them like we treated Emily? Is it because young kids are difficult to treat? Or maybe we’re trying to eliminate the headache of doing two phases? Or is it that we haven’t figured out a way to monetize Phase I treatment? Maybe it’s because we were never taught how to provide effective interceptive treatment?
Whatever the reason, I encourage you to keep an open mind towards interceptive treatment. Certainly not every patient needs Phase I. But our job as diagnosticians and clinicians is to determine who could benefit from it, and then provide painless, efficient, and effective interceptive treatment to those patients. And when you do Phase I, please make sure you get the anterior teeth straight, so the patient has a smile they are confident in. After all, you just never know whose life you’re going to change!
For more information on the amazing benefits of well-timed and well executed interceptive treatment, including its impact on airway, be sure to check out the 2-part series of The DOC Podcast titled A Paradigm Shift in our Approach to Interceptive Treatment (Part 1 & Part II) and take the DOC CE Course titled Airway, Malocclusion, and Interceptive Orthodontic Treatment which provides 4.5 ADA CERP-recognized CE hours!